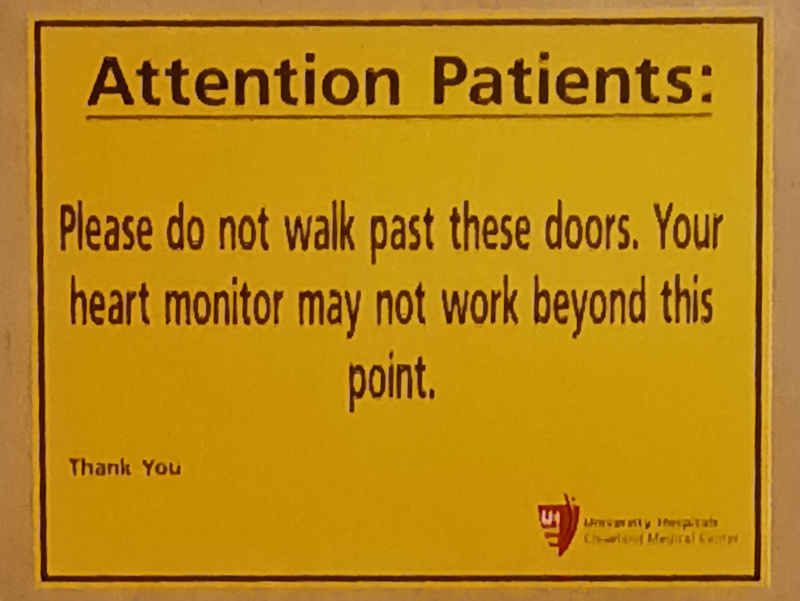
In this third and final blog post about my December 2022 through spring 2023 experiences with hypertrophic cardiomyopathy (HCM), I share information about my week on the University Hospitals third floor in both the Cardiothoracic ICU (intensive care unit), and then the post-surgical telemetry unit. I end the blog post writing about my first week and month at home.
If you have not read my first two HCM blog posts, I invite you to learn more about my experience in:
After Surgery on Thursday, April 27, 2023
Hospital Stay Through Thursday, May 4, 2023
Evening of the procedure [from University Hospitals SeamlessMD]
What will I look like when I wake up?
When you wake up, you will notice that some wires and tubes from the procedure are still on you. They will be attached to machines by your bed. Each item helps to keep you safe.
Some tools attached to you may include:
- A breathing tube in your throat. This tube is connected to a ventilator (breathing machine) to help you breathe. Most people do not notice the tube due to the anesthesia (sleeping medicine). This will be removed a few hours after surgery.
- Intravenous (IV) lines. You may have more than 1 IV line, including 1 on your neck and 1 on your wrist. These tubes are used to give you medicine and liquids.
- A tube in your chest. This tube will remove any liquid from your procedure.
- Urinary catheter. It drains the pee from your bladder.
- Leg squeezing devices on your leg. This will help with blood flow.
- Other wires will be attached to you to monitor your blood pressure, heart rate, and breathing.
If your breathing tube is in, you will not be able to talk. Nod your head yes or no to answer questions.
The whole time I was in the hospital, I left my iPhone in airplane mode, and except for one night rewatching the movie Men in Black: International, I never turned on the television. I chose to be totally disconnected from anything outside of my hospital room, and lived only in the present during this first week of post-surgery recovery. (My wife, Julie, did receive emails with my health recommendation notices from the University Hospitals SeamlessMD website, and updated family and friends about my status via email and social media.)
It is interesting how my progress was not linear -- I had bad times after good. My strength and pain came and went away with no logical relation to what I was doing. Starting even the first evening, I found that sitting was better then lying down. Being in what you would expect to be resting postions actually was more painful. After the first day, walking and sitting were better for me than lying down -- lying down to sleep led to waking in more pain.
The fourth day after surgery (Monday, May 1, 2023), I did turn on my iPhone to jot down some notes about my experiences for this blog post, which I later edited to create the following:
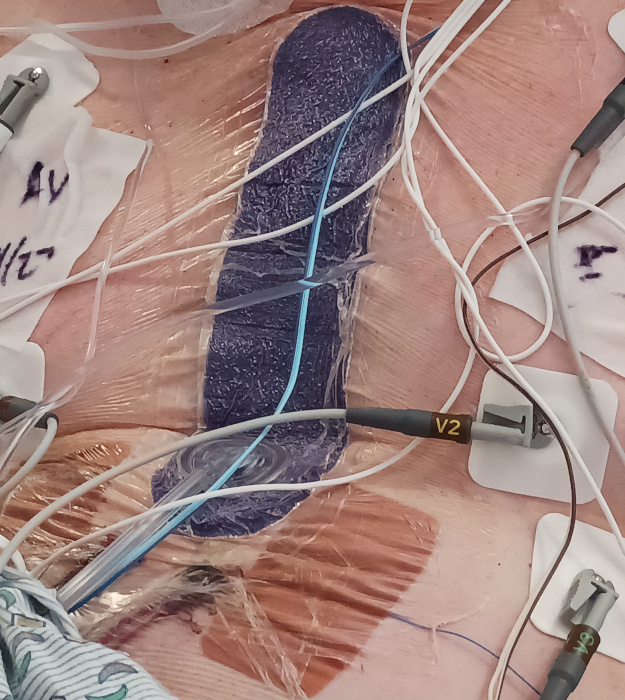
Negative air pressure patch over chest wound
I found in my bag after my surgery papers with information about the PREVENA™ Therapy system by KCI, so I assume the following video and press release describes a similar system to what was used after my surgery. Note that the video was published May 9, 2023, which was after my surgery date.
One thing I had not read about before my surgery was the technique of having the chest opening covered with a patch that is attached to an air pump that keeps negative air pressure on the wound. The device I wore for several days was very noisy, but I told the nurses that the noise did not bother me if it was helping me heal faster. Having this patch over my chest also meant that I did not get to see how large the chest wound was until about five days after my surgery. I was prepared for the scar to look worse than it did when I finally saw it.
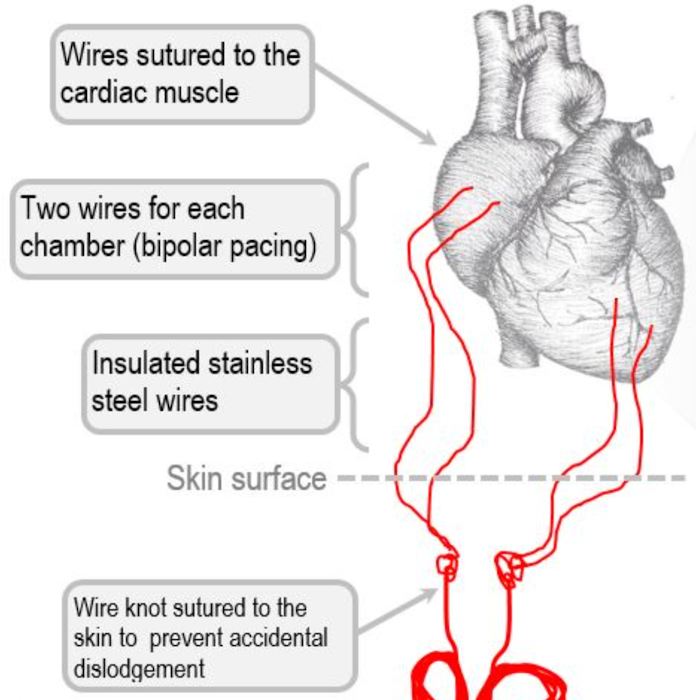
Temporary Pacemaker
Before my surgery, I had learned about the use of a temporary pacemaker, but how it was actually used was not at all what I expected!
I had a temporary pacemaker which was not used, but was always there and ready if needed. After the second day, a nurse practitioner turned off the control box attached to the pacemaker, and on the fifth day, which was Tuesday, May 2, 2023, they took away the box entirely. I was told that the wires going to my heart would be the last thing removed before I left the hospital.
Actually, I later learned that most of the two sets of wires would never be removed, that instead they would be left inside my chest. Only the parts on the outside of my body would be removed. It was very odd to watch the wires on the outside be cut and then the rest slip into my body.
In the future, if I ever have another MRI, I will need to tell the MRI technician about my “retained epicardial pacing wires.” It is strange to think that I will have these wires inside my chest area for the rest of my life.
Here is a close-up photo of one of the two devices taped to my body as part of the temporary pacemaker. Wires from this device led directly to one side of my heart while the other one went to the other side of my heart.
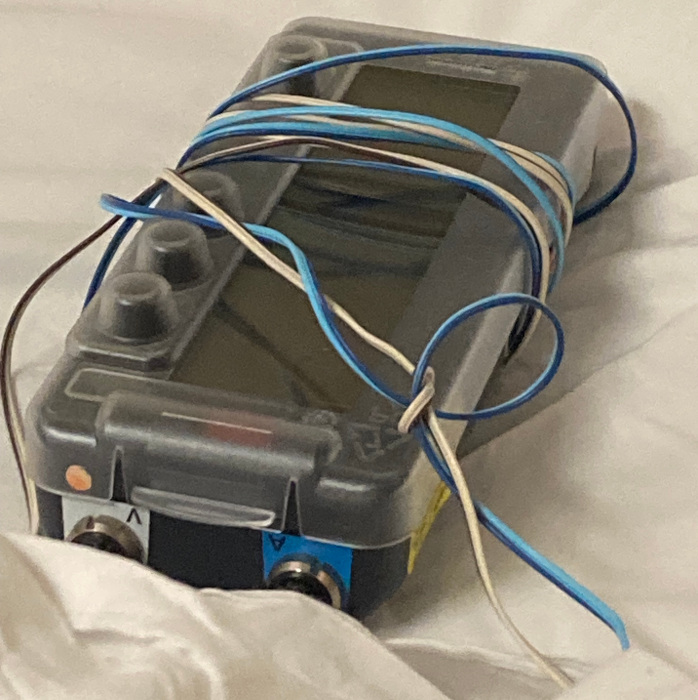
Here is a photo of the temporary pacemaker controller that connected to the two sets of devices taped to my body. After the first day, the controls were turned off, and I had to carry this heavy box around for most of the time I was in the hospital.
Intermittent Pneumatic Compression Device
I wore inflatable leg sleeves whenever I was in bed (which for me was only in the night, since I was more comfortable sitting in a chair). I was familiar with Intermittent Pneumatic Compression Devices from when other family members were in the hospital, and I welcomed the opportunity to always wear them when in bed. The idea of getting a blood clot scared me -- I didn't mind having my legs in these sleeves all night while I try to sleep.
Pain Levels from 0 to 8
Immediately after surgery, I didn’t feel much pain, since I chose to have a nerve block administered while I was under anesthesia. The next two days, I had a very high level of pain for half of each of the days.
I couldn’t really walk the first day, but joked with the hospital staff that even though I wanted to walk that evening, I couldn't due to the large number of wires and tubes attached to my body.
Uncomfortably Numb
My right hand was completely numb when I woke after the surgery. I was told that the numbness was probably due to a nerve being pinched from the position my right hand was in for the hours of surgery.
On Sunday, which would be recovery day three, the thumb and first two fingers (pointer finger and middle finger) gained full sensation back again, but the other two fingers on the right hand (pinky and ring finger) still felt numb the entire time I was in the hospital and for weeks at home. I have been told that the feeling in these two fingers and the base of my hand will come back --- hopefully in a few months.
Echocardiogram, Chest X-ray, EKG
ECHOCARDIOGRAM [for Stuart O. Smith, Jr.]
Collected on April 28, 2023 4:43 PM. . . .
In comparison to the previous echocardiogram(s): Compared with study from 3/31/2023,. LVOT gradient is now reduced post myectomy to 20mmHg from 35mmHg.
I was given an EKG and echocardiogram to confirm that my pain the first two days after the surgery was not from other issues, and the results were good. Plus, the added good news from the echocardiogram is that it showed that my surgery was successful in lowering my LVOT (left ventricular outflow tract) gradient!!
I was surprised that I had a chest x-ray taken in my room every day, and one time they took my to a lower floor to take chest x-rays with me standing for a side view.
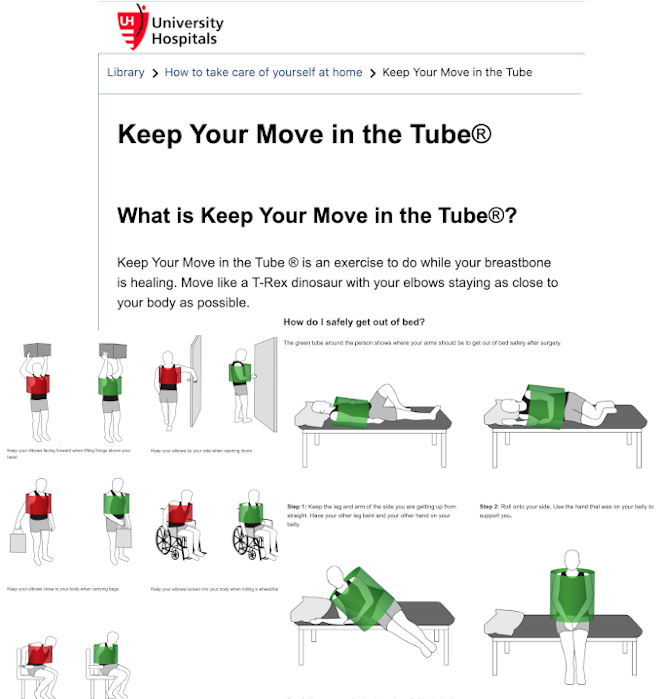
Keep Your Move in the Tube®
I was terrible at keeping my moves in the tube when getting in and out of bed at the hospital. I guess I am just not a good T-Rex dinosaur. Here are two videos that you can share on why it is effective to "keep your move in the tube®," and how it should be done correctly:
Walking
I was told by a nurse on Sunday, April 30, 2023 (third day after surgery), that I was walking more than other patients on this floor. Despite my early success with walking, however, I found that later in the week, I had bad times where I felt too exhausted to do much walking at all.
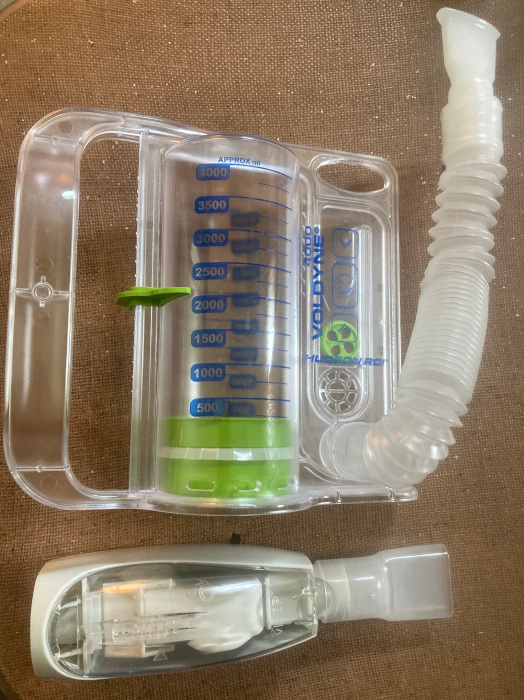
Incentive Spirometer (Inhaling) and a Blowing Exercise Device (Exhaling)
In addition to walking, I was told that using the two breathing exercise devices that I was given would help my lungs return to normal. Having both my lungs and heart completely stopped during surgery required work post-surgery to keep my lungs healthy.
Before my surgery, I had read on University Hospitals SeamlessMD that I should "Do [my] breathing exercises 10 times every hour" while in the hospital, and also to continue after I get home. While there were many hours I missed while in the hospital, since I was asleep from exhaustion, the hours I did do both the inhaling and exhaling breathing exercises, I always did them 20 times. I figured if doing ten was good, then doing 20 would help me get healthier faster.
12 O’clock Midnight -- HTML 3-D Chest Pain Dream
A nurse woke me around 12 o’clock midnight Sunday/Monday, to give me medicine. Since I was woken mid-dream, I remember my very strange dream that I was designing an HTML 3-D representation of the pain in my chest. Yes, the pain got into my dream as a three dimensional vision!
Weight Gain
After the first couple of days, I was weighed every morning. I was alarmed by the weight gain that I saw every day that it was checked in the hospital. I was told that the weight gain was due to fluid retention.
Cracking Sound From Breast Bone
Before my surgery, I was told via the University Hospitals SeamlessMD app that hearing/feeling a cracking sound/pain in my chest was normal. Even knowing in advance about this, it was still concerning every time I felt it -- it is not a normal feeling!!! I look forward to the day in several months when my chest bone is fully grown back together!
Tuesday, Wednesday, Thursday - Three Days I Almost Went Home
For three days, I was told that I was doing really well walking and being active, and that I would be able to go home. All three days had something come up.
I was fine with staying longer in the hospital (if needed), since I only want to do what is best for the long-term outcome. I do have to say that it felt weird waking up Thursday morning to have breakfast again in the hospital, remembering that one week earlier I was preparing for my surgery at that time.
TED Hose
One item was out of sync with the University Hospitals SeamlessMD website that my wife was checking for me. I received the following "May 2 2023 -- Missed these targets" notice from SeamlessMD:
I was not concerned about the compression stockings, since despite gaining fluid weight, my legs were looking quite normal for the five days after my surgery, and I was walking. That all changed on day six (Wednesday, April 3, 2023), when I was talking to a nurse practitioner about going home. We both noticed that my legs had suddenly swollen overnight, which delayed my discharge from the hospital. I wore TED hose from that date through Tuesday, April 16, 2023, when the swelling finally went away after a week and a half at home.
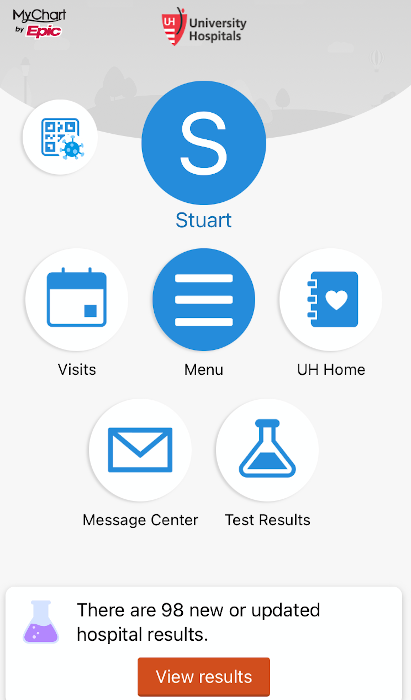
Turned on iPhone UH MyChart Health App — 98 Notifications
After I was told that I was finally going home on Thursday, May 4, I turned on my iPhone to see the huge number of notifications from the University Hospitals health apps. The new University Hospitals MyChart app stated that I had 98 new hospital test results.
Starting Thursday, May 4, 2023 - First Week at Home
I’m glad to be going home today after having my heart repaired with a septal myectomy at @UHhospitals Harrington Heart & Vascular Institute @HarringtonHVI
— Stuart O. Smith, Jr. - sosAssociates.com (@sos_jr) May 4, 2023
A genetic heart disease, Hypertrophic Cardiomyopathy (HCM) negatively impacted my quality of life for the last 4 months. pic.twitter.com/TVh5Ycc8VN
What to expect week 1 at home [from University Hospitals SeamlessMD]
Try to:
- Eat a heart-healthy diet
- Drink enough liquids
- Do your breathing exercises every hour
- Walk at least 4 times every day for 5 to 10 minutes
- Rest your body
- Protect your chest
- Keep your legs raised when you are sitting or lying down
- Take your medicines as prescribed by your doctor
- Shower and clean your wound every day
- Fill out your Health Check every day on this program [University Hospitals SeamlessMD].
- Be ready to talk to your nurse over the phone
It is normal to:
- Have some pain
- Have some trouble breathing
- Feel tired
- Have some redness and bruising around your incision
- See a little blood on your bandage
If you notice any problems, fill out a daily Health Check. We can tell you if these signs are normal or signs of trouble.
After four months of hypertrophic cardiomyopathy symptoms preventing me from walking any distance without being out of breath, the biggest difference for me getting home was the ability to walk farther in the park. While my walks were slow and for just under a mile with some heavy breathing, it still was great to be able to be outside again. Once the two halves of my sternum heal back together so I can lift some weight again, and my stamina returns, I plan to return to backpacking. This healing process will take several months.
Here are tweets about some of the park walks I was able to do my first week home from the hospital. I am grateful to all those people who replied to what I shared on social media with their well wishes now that I am back home.
Day One (First Full Day Home): Friday, May 5, 2023
- North Chagrin Reservation, Cleveland Metroparks
- Loop: North Chagrin Nature Center > Marsh Boardwalk > Buttermilk Falls Trail > All Purpose Trail
- Approximately 0.8+ miles estimated via the Gaia GPS iPhone app
#Cleveland Metroparks: “Water…Rushing Through Time”
— Stuart O. Smith, Jr. - sosAssociates.com (@sos_jr) May 5, 2023
After having HCM heart disease negatively impacted my quality of life for the last 4 months, it was great to be able to finally take a walk in @CleveMetroparks after being released yesterday from @UHhospitals @HarringtonHVI pic.twitter.com/SMyGB3d5ZP
I'm so glad to see you are feeling better
— (((clevecarole))) (@Clevecarole) May 6, 2023
Thank you, @Clevecarole. I’m looking forward to moving down the road of recovery .
— Stuart O. Smith, Jr. - sosAssociates.com (@sos_jr) May 6, 2023
You are on your way...
— (((clevecarole))) (@Clevecarole) May 6, 2023
Glad you're able to get out for a bit, Stuart!
— Brad Nellis (@Brad_Nellis) May 6, 2023
Thanks, @Brad_Nellis.
— Stuart O. Smith, Jr. - sosAssociates.com (@sos_jr) May 6, 2023
The walk yesterday went much better than expected, but I need to remember that everyday might be different.
You’re feeling pretty good then? I’m glad.
— Stacy (@jukebox65) May 5, 2023
Thank you, @jukebox65.
— Stuart O. Smith, Jr. - sosAssociates.com (@sos_jr) May 5, 2023
Post surgery pain management can be complicated. I try to take it hour by hour.
Today, so far, I have had several good hours together. I have several months to go before full recovery.
Best wishes Stuart. I’m sure you will be back to the trails fully soon.
— Stacy (@jukebox65) May 5, 2023
Thank you so much, @jukebox65!
— Stuart O. Smith, Jr. - sosAssociates.com (@sos_jr) May 5, 2023
Day Two Home: Saturday, May 6, 2023
- Euclid Creek Reservation, Cleveland Metroparks
- Upper level of the Eastern Ledge Trail (Donna Drive to overlook and back.)
- Approximately 0.8+ miles estimated via the Gaia GPS iPhone app
Looking for an easy level trail with great overlook?
— Stuart O. Smith, Jr. - sosAssociates.com (@sos_jr) May 6, 2023
I highly recommend the upper level of the @CleveMetroparks Eastern Ledge Trail via the connection trail off Donna Drive.https://t.co/ZPsAC56Puu
This is a new #Cleveland #Metroparks trail: https://t.co/PZ9fIg9JpM https://t.co/XwSqpjmAA7 pic.twitter.com/Wl9GGJ7FOV
Upper level of the @CleveMetroparks Eastern Ledge Trail is easily reached via connection trail to the city of Richmond Heights off Donna Drive at: 41.54699, -81.52047https://t.co/KpDzbiDJBW
— Stuart O. Smith, Jr. - sosAssociates.com (@sos_jr) May 6, 2023
The overlook: 41.54881, -81.52746 https://t.co/fLWi9uRtrb
GPS via @GaiaGPS #map app. https://t.co/mPtayHtEvp pic.twitter.com/0ZCU1vrep8
I was wondering how to get up there.
— Polly Karr (@karr_pe) May 6, 2023
@karr_pe, for level trail park on Donna Drive
— Stuart O. Smith, Jr. - sosAssociates.com (@sos_jr) May 6, 2023
41.54699, -81.52047https://t.co/KpDzbiDJBW
0.4 miles walk back to overlook.
If you don’t need the level trail, the new Eastern Ledge Trail up the steep hill is great!
Start at Euclid Creek Park Pavilionhttps://t.co/PKvLEEje1d
Thanks!
— Polly Karr (@karr_pe) May 6, 2023
Never heard of that, looks cool. I just discovered a cool spot in Berea. The sign at the start of the trail said "No Trail" so you know it had to be good. (Signs are for people who obey signs.)
— Eclipse Over Cleveland (@EclipseOverCLE) May 7, 2023
Day Four Home: Monday, May 8, 2023
- Euclid Beach in the Euclid Creek Reservation, Cleveland Metroparks
- Euclid Beach parking lot > Euclid Beach Pier > Cleveland Script Sign at Villa Angela Beach > and back
- Approximately 0.6+ miles estimated via the Gaia GPS iPhone app
I want to invite you to learn more about Cleveland Metroparks' Euclid Beach, the Euclid Beach Park Grand Carousel at the Western Reserve Historical Society's Cleveland History Center, and the historic Cleveland amusement park that closed in 1969 in my "Euclid Beach Park" blog posts. My son, Kevin, and wife, Julie, work to preserve this part of Cleveland's history as Board Members of Euclid Beach Park Now.
After having my heart repaired at @UHhospitals Harrington Heart & Vascular Institute @HarringtonHVI, I have been enjoying being able to take walks in our local parks again.
— Stuart O. Smith, Jr. - sosAssociates.com (@sos_jr) May 8, 2023
Today, I enjoyed a sunny #Cleveland view of #LakeErie from @CleveMetroparks’ #EuclidBeachPark Pier. pic.twitter.com/8zntcxQeey
@CleveMetroparks’ #EuclidBeachPark Pier.
— Stuart O. Smith, Jr. - sosAssociates.com (@sos_jr) May 8, 2023
The pier was built through the generous support of the @CleveFoundation, the @CleveMetroparks Emerald Necklace Endowment Fund, and the @OhioDNR.https://t.co/gjNjeKhD8khttps://t.co/MICtrtcdkj pic.twitter.com/bkWlobNVyB
I received a get-well message on Twitter from @CleveFoundation:
(Learn about what the Cleveland Foundation supports in our community in my blog posts here.)
#EuclidBeachPark 1895 - 1969 https://t.co/7MyHHbMzXL#Cleveland’s #EuclidBeachAmusementPark closed in 1969. Remnants of the beachside fountain and concrete footers of the Flying Turns roller coaster are still visible in this @CleveMetroparks. https://t.co/MICtrtcdkj pic.twitter.com/RBDclTy3U9
— Stuart O. Smith, Jr. - sosAssociates.com (@sos_jr) May 8, 2023
The …land! @TheCLE pic.twitter.com/pVKtPnbdmQ
— Stuart O. Smith, Jr. - sosAssociates.com (@sos_jr) May 8, 2023
Glad you're doing well. I must come see this. I was on all of those rides many times.
— Beverly Kristy (@KristyBeverly) May 9, 2023
@KristyBeverly, yes, you must visit @CleveMetroparks #EuclidBeach the next time you visit #Cleveland. The park has signs with historic info about the #AmusementPark.
— Stuart O. Smith, Jr. - sosAssociates.com (@sos_jr) May 13, 2023
I would also recommend you visit the Euclid Beach Grand Carousel at @CleStartsHere.🎠https://t.co/QsnF0PTrwq pic.twitter.com/Iol2LSl9br
We did the carousel with my grandkids 2 years ago. it's in beautiful shape.
— Beverly Kristy (@KristyBeverly) May 13, 2023
My wife & son are on the Euclid Beach Park Now Board.
— Stuart O. Smith, Jr. - sosAssociates.com (@sos_jr) May 13, 2023
My wife was at a board meeting tonight & recommends these events:
5/19 Grand Carousel Birthday Party🎠
7/22-23 Euclid Beach Park Days
9/24 Sights & Sounds of Euclid Beach Parkhttps://t.co/OEU6u2L6DAhttps://t.co/plbegLEXsF pic.twitter.com/GBCDNPnXLr
Thanks!
— Beverly Kristy (@KristyBeverly) May 13, 2023
If you're able, I recommend adding cycling to your health regimen. I have often cycled to Euclid Beach from my house in Old Brooklyn. A great ride!
— Eclipse Over Cleveland (@EclipseOverCLE) May 9, 2023
@EclipseOverCLE, oh I do have cycling plans once my chest bone heals, but currently I can’t risk the occasional need to lift the bike. Thanks for the suggestion for an interesting route for my future. https://t.co/AppCMiFwPQ
— Stuart O. Smith, Jr. - sosAssociates.com (@sos_jr) May 9, 2023
I gather Ohio has more miles of bike trails than any other state. So many around Cleveland, especially in the last 5 years. The Towpath, the many Metroparks trails, the Lakefront (to Euclid Beach). Fun, relaxing and healthful. Hope you heal up soon!
— Eclipse Over Cleveland (@EclipseOverCLE) May 9, 2023
Nice! Glad you’re feeling better- my summer hang out! Thanks for showcasing my #Collinwood neighborhood #EuclidBeach https://t.co/aBfcHegpGi
— ToniChanakas (@tonichanakas) May 9, 2023
Did you notice EB Park homes don’t impede access to Lake Erie?
— Andre' Dailey (@AndreDaileyCLE) May 9, 2023
@AndreDaileyCLE, yes, I noticed.
— Stuart O. Smith, Jr. - sosAssociates.com (@sos_jr) May 9, 2023
Sunday, June 4, 2023 - Review of First Month at Home: Patience Required!
After the first week at home (May 4-11, 2023), issues arose that seriously slowed me down. Apparently, my successful first week of feeling energetic enough to walk was not the norm. Very similar to my experience in the hospital, my progress was not linear -- I had bad times after good.
It is hard to explain -- at the same time I felt so much better than I had for the first four months of this year with my hypertrophic cardiomyopathy symptoms, I now had problems caused by the after-effects of the surgery. The debilitating symptoms from having a deformed heart caused by HCM were eliminated by the surgery, but the surgery caused the following issues:
The results of the Thursday, May 11, 2023, blood test showed that my number of red blood cells was down (Anemia). This was the biggest problem for me during the first month at home -- always feeling fatigued and sometimes chilly. I have never been a person who gets cold, but now I often need a blanket -- I became a real "freeze baby." So while my brain, heart, and lungs were ready to be active again, I had to be patient and give my bone marrow time to replace all the blood lost during surgery. I was told that it could take a couple of months for the fatigue to go away.
On Saturday, May 20, 2023, the glue that held the top part of my chest wound together started to loosen and then came off. It was like having a zipper open up my chest. I was told over the phone to let the wound air dry and use Betadine to try and prevent infection. On Wednesday, May 24th, I met with a surgeon, and she confirmed that the now open wound was mildly infected. I started taking antibiotics for five days, and to pack the wound with wet-to-dry dressings at least twice a day. It sometimes hurts to move due to the dressing, and the changing of the dressing is not fun -- it is a bloody mess. With this open chest wound, I will now have a larger scar on my chest. It is also strange to see the blue thread (surgical sutures) that was to be inside me holding my body together now exposed in the deeper part of my chest wound. It will take a long time for the wound to fill in with new, healthy tissue -- I must be patient!
The right side of my right hand continues to feel numb. Also, my left hand now often falls asleep when it is elevated -- this is a new issue!! It is hard not to lose patience waiting for my right hand nerves to return to normal. When typing and washing hands, it feels very strange to have no feeling in part of my right hand.
The good news is that despite not being as active as I had planned, I am emotionally in good spirits and looking forward to my return to normal health in a few months. When I met with my cardiologist, Dr. Gorodeski, on Tuesday, May 16, 2023, to check my wound and blood test results, he told me that it is common for patients to have severe depression after open heart surgery. Apparently, stopping both your heart and lungs can impact your brain -- this makes sense! I only mention this here so that others know to get/offer emotional help if needed after open heart surgery.
More good news came via a phone call. My surgery was on Thursday, April 27, 2023, and on Friday, May 26, 2023, I received a call from a nurse in the University hospitals surgery department to see how I was doing. She let me know that the first month is the highest risk for post-open-heart-surgery patients needing to return to the hospital. With help, I had successfully stayed in my home with no serious issues. I believe this means my prognosis is good for my full recovery if I remember to be patient and continue to take care of myself.
I had a special “wound check” appointment today.
— Stuart O. Smith, Jr. - sosAssociates.com (@sos_jr) May 24, 2023
The doctor said that it was good that I came in when she saw my wound. She said I caught a problem before it got serious.
I have a follow-up appointment with my surgeon next week. pic.twitter.com/1U6JWczoVw
Take care Stuart!
— (((clevecarole))) (@Clevecarole) May 25, 2023
@Clevecarole, thanks! Yes, I am taking care of myself.
— Stuart O. Smith, Jr. - sosAssociates.com (@sos_jr) May 25, 2023
Last minute change.
— Stuart O. Smith, Jr. - sosAssociates.com (@sos_jr) June 2, 2023
My surgeon had an heart transplant scheduled today at the last minute, and had to cancel my appointment.
Instead I had a virtual "wound check" appointment with another doctor & my surgeon's nurse.
My wound looks better, and I will meet in-person next week. pic.twitter.com/fNiQYSwfey
University Hospitals SeamlessMD final message:
Saturday, June 3, 2023, was the "end of program" day (30 days home) for University Hospitals' SeamlessMD and also happened to be 2023 National Trails Day®. Last year, I wrote the following blog post about my participation in the Buckeye Trail Association's National Trails Day® event:
Blog Date: June 15, 2022 - National Trails Day 2022: Buckeye Trail Association's Biggest Day Hike
"It feels appropriate that the first blog post I am writing since my Continental Divide Trail backpacking adventure in April 2022 is about a National Trails Day® event . . ."
Today's message from @UHhospitals’ @SeamlessMD:
— Stuart O. Smith, Jr. - sosAssociates.com (@sos_jr) June 3, 2023
“Hi Stuart,
You have finished your at-home recovery program!”
“We hope you have found this online program helpful!”
“This program ends 30 days after you go home”
“We wish you all the best in your healthcare journey!” pic.twitter.com/uFSMF2QfWt
Here are some tweets about the 2023 National Trails Day®. Since I was still recovering from surgery, I did not participate this year, but I look forward to future years! My decision to have surgery to treat my Hypertrophic Cardiomyopathy will enable me to return to the trail!
Happy #NationalTrailsDay23! #CDT
— Continental Divide Trail Coalition (@CDNST1) June 3, 2023
Today is the last chance to enter to win a free Osprey Tempest pack as part of our Take Action for Trails week! Find details here: https://t.co/Dod2n9K7Qf
Ryan Lim pic.twitter.com/ULEKW9c0Ie
SATURDAY IS JUST A FEW DAYS AWAY which means the Biggest Day Hike 2023 is almost here! Don’t forget to register your hike/bike/paddle/trail ride!
— The Buckeye Trail (@hikethebt) June 1, 2023
Let's see how much of the Buckeye Trail we can hike together.
For more information and to register visit: https://t.co/L33ZuQY3Xd pic.twitter.com/yUiqbNXLhF
Today is #NationalTrailsDay, and we're celebrating the Appalachian Trail and the community of people who love and care for it.
— Appalachian Trail Conservancy (@AT_Conservancy) June 3, 2023
Christopher "WeatherMan" MacArthur pic.twitter.com/yuohnmgG4I
Please consider donating to protect the A.T. forever and for all in honor of National Trails Day.
— Appalachian Trail Conservancy (@AT_Conservancy) June 3, 2023
Donate here: https://t.co/5hSrKdbx1h
Bonus: the first 100 people who become members, or renew their membership, with a donation of $50 or more will receive a limited edition ATC X BearVault weather-resistant trail journal!
— Appalachian Trail Conservancy (@AT_Conservancy) June 3, 2023
#NationalTrailsDay is Saturday, June 3! This annual day of service started by our friends at @AmericanHiking is the perfect opportunity to visit and give back to trails.
— Rails-to-Trails Conservancy (@railstotrails) June 1, 2023
Explore events + ways to participate at https://t.co/v5Pk2Xvt1i! https://t.co/38IwfsIdYJ
Happy National Trails Day! Whether you're participating in the @hikethebt Biggest Day Hike or are just hitting the trails in your favorite State Park, take a moment to enjoy the trails & all they have to offer! Happy hiking, biking & riding!#nationaltrailsday #ohiostateparks pic.twitter.com/WAcZ23zTHn
— Ohio State Parks & Watercraft (@OHStateParks) June 3, 2023
It’s @AmericanHiking #NationalTrailsDay!
— American Hiking (@AmericanHiking) June 3, 2023
Join the nationwide movement to give back to trails and connect with the people in your community who share a love of being outside! pic.twitter.com/aaaQRi4gqk
Take the National Trails Day® pledge to leave the trails & outdoor community better than you found them https://t.co/6KekPfNryE
— American Hiking (@AmericanHiking) June 3, 2023
Taking the pledge enters you to win one of four prize packs worth more than $1500! *You have until 6/5 to take the pledge, winners announced 6/12!
National Trails Day® is made possible by: Apparel Sponsor AKHG by @DuluthTradingCo, Premier Beer Sponsor @AthleticBrewing, @REI, @OspreyPacks, Waterford Press, LOWA, @Fjallraven_NA, @GORETEXna & federal partners, @NatlParkService, @forestservice, @USFWS, @BLMNational & @USDOTFHWA
— American Hiking (@AmericanHiking) June 3, 2023
On this #InternationalTrailsDay, there’s a lot going on! As part of our Trail Care Grant Program, several trail groups across Canada are cleaning up, enhancing and improving their local trails! Thank you to all the dedicated volunteers for your amazing work! 🫶🏻 pic.twitter.com/KlTapViDgK
— Trans Canada Trail (@TCTrail) June 3, 2023
En cette #JournéeInternationaledesSentiers, ça bouge! Dans le cadre du Programme de subvention de La grande corvée, plusieurs groupes de sentiers à travers le pays nettoient et améliorent leurs sentiers locaux! Merci à tous les bénévoles pour votre incroyable travail! 🫶🏻 pic.twitter.com/465yhFR0F2
— Sentier Transcanadien (@SentierTC) June 3, 2023
Lace-up your boots 'cause it's #NationalTrailsDay!
— AllTrails (@AllTrails) June 3, 2023
Tell us your go-to trail in the comments below
PS: Tag us in your adventures using @alltrails #alltrails for a chance to be featured!
@physiopham
@shot_bybenhttps://t.co/E2wkNjSTMI pic.twitter.com/X9kteCn04Q
#NationalTrailsDay pic.twitter.com/1vQsOd6mne
— National Park Service (@NatlParkService) June 3, 2023
Find the trail for you at: https://t.co/AcVkeTKjb6
— National Park Service (@NatlParkService) June 3, 2023
Hypertrophic Cardiomyopathy is a Progressive Heart Disease
With the completion of my septal myectomy surgery, I am looking forward to returning to my normal active life once I recover from the open-heart surgery. At the same time, I know that I have hypertrophic cardiomyopathy (HCM), which means that I need to be prepared for future changes to my heart. The surgery to remove a small part of the thickened muscle between the heart chambers should be a permanent solution to the HCM symptoms I had the for the first four months of the year, but I will need to be on the watch for other issues.
I have been told that hypertrophic cardiomyopathy is a progressive disease — the heart will continue to stiffen. I will need regular check-ups with my cardiologist, which will include an echocardiogram and EKG. I will also need to wear a heart monitor for a couple of weeks every year to confirm that my cardiac electrical system is still functioning correctly.
With hypertrophic cardiomyopathy being a genetically caused heart disease, my blood relatives will also need to be on the watch for symptoms and should seriously consider getting HCM genetic testing.
Fourth HCM Blog Post??
As I was writing the outline for these three HCM blog posts, I also envisioned a potential fourth blog post entitled: My Hypertrophic Cardiomyopathy Part Four: Recovery, which would be about normal life after I am fully recovered from my early 2023 symptoms. At this point, I doubt I will write a fourth blog post, but know that all future blog posts about my having a normal life will be made possible due to the diagnosis and treatment I received from the doctors and nurses of University Hospitals.
If you have not read the first two HCM blog posts, please see:
Comments
My HCM Part Four: Recovery & A.T. Hike Featured on WKYC TV-3
Submitted by Stuart Smith on Tue, 01/02/2024 - 15:09

Stuart O. Smith, Jr., MNO
Blogging at: sosAssociates.com/Blog
Former Cleveland GiveCamp Steering Committee: ClevelandGiveCamp.org/about/#steering
Former Web SIG Cleveland Leader: WebSigCleveland.org



On June 11, 2023, I ended my third Hypertrophic Cardiomyopathy (HCM) blog post questioning whether I would have a fourth "recovery" blog post. Well, my idea of writing an HCM recovery blog post changed from a doubt to a must-do when on October 16, 2023, my cardiologist, Eiran Gorodeski MD, MPH, recommended I share on television my story about backpacking on the Appalachian Trail after my open-heart surgery. This led me to meet with TV-3 News Special Projects Reporter Lindsay Buckingham on December 5, 2023, at a special location.
In this recovery blog post, I shared an update on the great progress I have made, information about the significance of the interview's location, and then the actual interview that was broadcast, along with its companion article.
Please read this recovery blog post: